Abstract
Introduction: PCNSL is a rare malignant tumor arising in the brain, spinal cord, eyes, or leptomeninges. HD-MTX-based regimens remain the first option for newly diagnosed PCNSL because of high response rates as demonstrated by numerous studies (Qing et al. Cancer Manag Res 2021). Bruton's tyrosine kinase (BTK) is a crucial part of the B-cell receptor signaling pathway, and BTK inhibition has been proven effective in treating CLL and other B-cell lymphomas (Yoshitaka et al. Neuro-Oncology 2021). Orelabrutinib is a newly developed BTK inhibitor with high selectivity and a high concentration in the cerebrospinal fluid (Zhang et al, EHA 2022). Recent evidence has shown the efficacy and safety of orelabrutinib in PCNSL (Wu et al., Invest New Drugs 2022). Therefore, we conducted a retrospective study of clinical outcomes in newly diagnosed PCNSL patients (pts) treated with orelabrutinib combined with rituximab and HD-MTX (RMO) regimen in routine clinical care.
Methods: This retrospective cohort included the pts (aged 18-80 years) with newly diagnosed PCNSL who received at least 2 cycles of RMO regimen (rituximab 375 mg/m2 iv day 1; MTX 3.5 g/m2 iv day1; orelabrutinib 150 mg qd po; 3 weeks per cycle) as the induction therapy in a real-world setting between May 2021 and June 2022. It was proposed to receive orelabrutinib monotherapy as maintenance after RMO therapy when deemed necessary. Efficacy was assessed by MRI/PET per the International PCNSL Collaborative Group (IPCG) criteria. The primary endpoint was overall response rate (ORR); secondary endpoints were CR rate, progression-free survival (PFS), overall survival (OS), and safety.
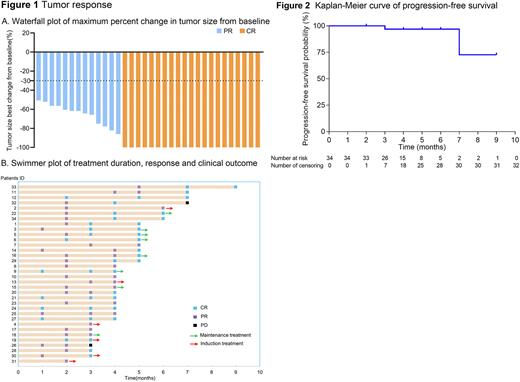
Results: Thirty-Four pts with newly diagnosed PCNSL (20 male; 24 non-GCB subtypes) were included, with a median age of 58.5 years (range: 30-79). Four (11.8%) pts had an ECOG performance status of ≥3. All the pts (100%) achieved certain responses (Figure 1) with a complete response in 21 pts (61.8%). Eighteen (52.9%) pts completed 6 cycles of RMO as induction, with an ORR of 94.44% (17/18) and CR rate of 88.89% (16/18) at the 6th cycle assessment. As of the cut-off date (June 30, 2022), 8 pts received orelabrutinib maintenance therapy and had a CR status. Median PFS was not reached (95% CI, 7 months-not reached; Figure 2), with a 6-month PFS rate of 97.0% (95% CI, 91.3%-100.0%). Median OS was not reached either. In 22 pts who were available for gene alterations profiling, 18 pts (81.8%, 18/22) had an MYD88 mutation and achieved an ORR of 100% (CR, 55.6%). Four of these 18 pts were found to have a mutation in CD79B simultaneously. Plasma and CSF samples were collected from 5 patients at 2 hours after 15-day consecutive administration of orelabrutinib. The median CSF concentration of orelabrutinib was 21.6 ng/ml (range, 15.9-48.5), and the median CSF/plasma free ratio was 58.6% (range, 38.6%-82.5%). All these 5 pts achieved a response (3 CR; 2 PR). Six of 34 (17.65%) pts experienced adverse events (AEs). The most common AE was white blood cell count decreased (8.82%). Only 2 (5.88%) pts experienced 4 ≥grade 3 AEs, including white blood cell count decreased, anemia, platelet count decreased, and alanine aminotransferase increased. No treatment-related death occurred.
Conclusion: This retrospective data suggested that orelabrutinib combined with RM had an encouraging anti-tumor activity in newly diagnosed PCNSL pts, with a toleratable safety profile. A prospective clinical trial is on the way to confirming this finding, and the results will be publicly disclosed after its completion.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal